How automating workflows in healthcare research ensures compliance instead of critical errors
Table of contents

Try Workflow Automation free for 14 days
In the world of healthcare research, science itself is, of course, important. But science is just one part of the equation. Behind every scientific breakthrough or clinical trial lies a mountain of documentation, disclosure requirements, and compliance processes — all of which are critical to maintaining ethical standards and regulatory approval.
The stakes in healthcare are extremely high. Not only can the administrative burden of managing documentation pull time and resources away from the work that really matters, but non-compliance and documentation errors can lead to serious consequences for research institutions, like rejected grant applications, suspended trials, or costly penalties.
Surprisingly, with the stakes so high, many healthcare research institutions still rely on manual, paper-based processes that aren’t only time-consuming and costly, but can increase the risk of error and non-compliance.
The good news? There’s a better way to manage these critical processes — one that increases efficiency, reduces administrative burden, and strengthens compliance.
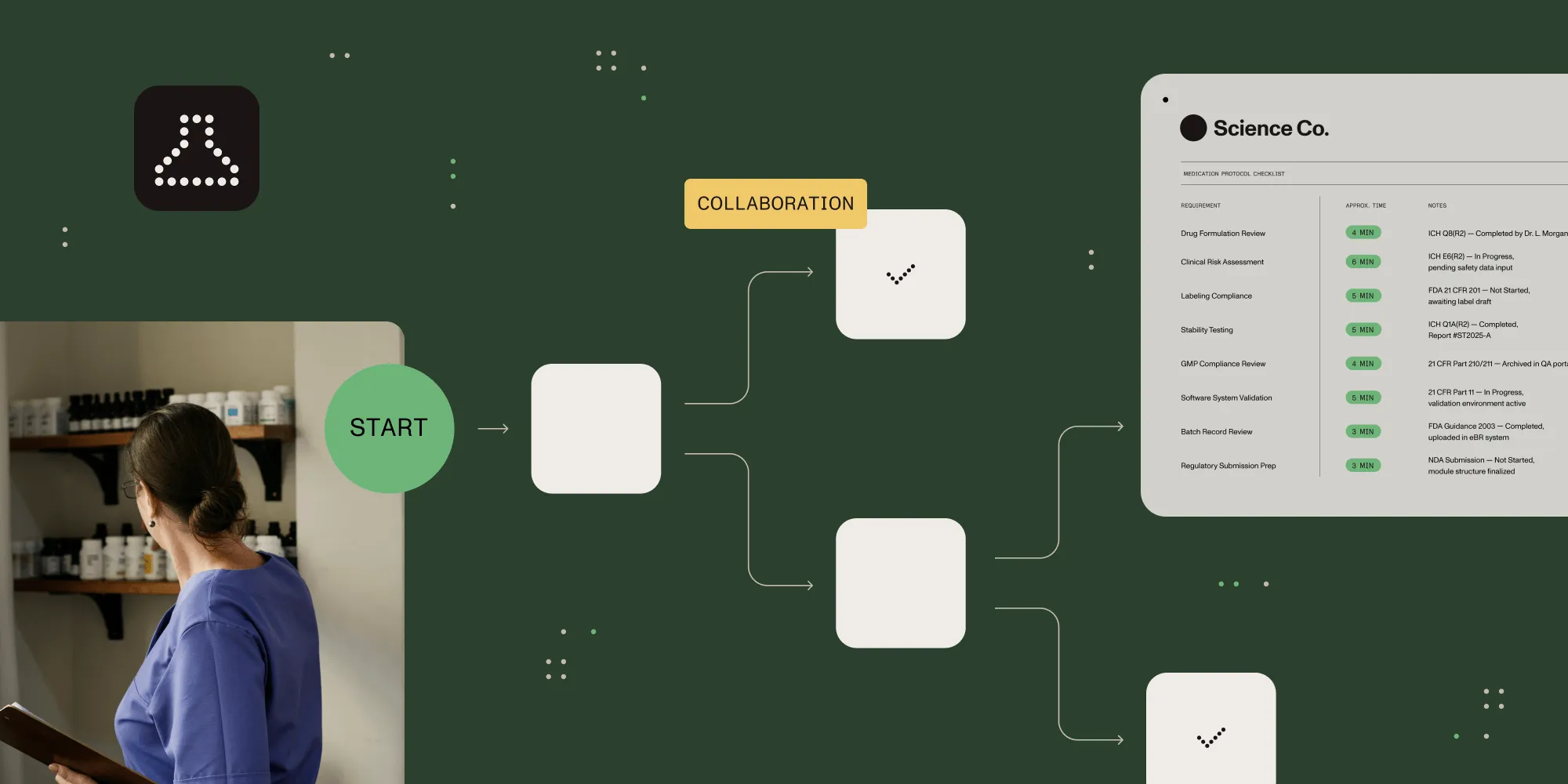
That better way is healthcare research workflow automation.
Healthcare workflow automation can revolutionize the way research institutions manage their documentation processes, which in turn can free up time and energy for their teams to focus on innovation.
But how exactly does healthcare research workflow automation work? What are the workflow challenges in the research world, and how do automated processes address those challenges? And how can you start implementing workflow automation within your organization while reaping all the rewards that go along with it?
The compliance maze: Understanding research workflow challenges
Before jumping into how automation can improve research compliance processes, first take a look at what makes these workflows so challenging to begin with.
Complex disclosure requirements
Healthcare research has complex and varied disclosure requirements, all of which require their own unique documentation workflows:
- Financial conflicts of interest — Researchers must disclose financial relationships with pharmaceutical companies, medical device manufacturers, and other entities that might influence their research. These disclosures might include consulting and speaking fees, equity interests, intellectual property rights, and other financial connections — all of which need regular updating and disclosure to institutions, journals, and funding agencies.
- Non-financial conflicts — Researchers must also disclose non-financial relationships that could influence their research, like advisory board positions, family connections to industry partners, or personal relationships.
- Protocol deviations — If researchers deviate from approved research protocols in any way, they need to document that deviation and report it to any relevant oversight committees. These reports must detail what happened, why it happened, what corrective actions were taken, and how similar deviations will be prevented in the future. Once the reports are complete, they then need to be submitted and tracked.
- Adverse events — Problems that come up during the research process need to be documented and reported within strict timelines and to all relevant parties. For example, IRBs, sponsors, and sometimes regulatory agencies like the U.S. Food and Drug Administration(opens in a new tab) (FDA) require reporting to include details about the event, severity, and relationship to the research.
Multiple stakeholders and approval pathways
Another challenge with healthcare research documentation workflows is that they typically involve multiple stakeholders — each with their own review and approval requirements. For example, healthcare research documentation may need review and approval from a variety of internal and external stakeholders.
- Institutional Review Boards (IRBs) — IRBs(opens in a new tab) are committees that review research protocols to ensure they meet ethical standards and protect human subjects. IRB submissions often require extensive documentation, including protocols, informed consent forms, and recruitment materials.
- Ethics committees — Beyond IRBs, and depending on the area of research, additional ethics reviews may be needed for specialized research areas like stem cells, genetic modification, or animal studies.
- Grant administrators — These professionals oversee compliance with funding agency requirements, ensuring disclosure reports, budget updates, and progress reports are submitted accurately and on time.
- Regulatory affairs specialists — In clinical research, regulatory affairs specialists ensure compliance with FDA regulations, international standards, and institutional policies. Additionally, they have their own unique and complex documentation requirements.
- Departmental reviewers — Research protocols and other documents often need internal departmental review and approval before moving to institutional or external stakeholder-level review.
- Sponsors — When research is sponsored, each sponsor often has their own documentation and reporting requirements, whether the sponsors are government agencies, pharmaceutical companies, or external foundations.
Changing regulatory landscape
Another challenge with healthcare research workflows is that research compliance is always evolving. With that evolution comes a host of ongoing regulatory, compliance, and documentation requirements.
- Regulation updates — Federal regulations — like the Common Rule(opens in a new tab), which regulates research that includes human subjects or participants — undergo periodic revisions. Whenever there’s a revision, institutions have to update their processes, forms, and workflows to comply with any relevant changes.
- Agency-specific requirements — In addition to federal regulations, independent funding agencies — for example, the National Institutes of Health (NIH), the National Science Foundation (NSF), or private foundations that focus on specific areas of research — may have their own disclosure and reporting requirements. These may also change over time, requiring research institutions to update their processes to ensure compliance.
- Institutional policy changes — In addition to external changes, internal policies may also evolve — both in response to external changes or institutional priorities, and for increasing efficiency or productivity — requiring updates to workflows and documentation.
- Location-based variations — For multisite or international research, teams must navigate different regulatory frameworks and requirements across the different states, regions, or countries in which they operate.
How manual processes increase research compliance challenges
Clearly, healthcare research workflows can be complex and can present a wide variety of challenges. If you’re still managing these processes — and all the documentation that goes along with them — manually, chances are you’re creating even more challenges that impact administrative efficiency, compliance, and your institution’s ability to innovate and complete research.
How? Manual processes further complicate healthcare research workflows in a multitude of ways, outlined in the following section.
Documentation inconsistencies and errors
It doesn’t matter how smart and organized your team and researchers are. They’re human, and humans make mistakes.
Having your team manually manage document workflows can create numerous opportunities for inconsistencies and errors, such as:
- Transcription errors — Manually moving information between systems — like from paper forms to electronic databases — increases the chance of mistakes, missing fields, or data entry mistakes. There may also be issues with interpreting handwriting, which can lead to incorrect data being entered into the system.
- Version control issues — In research, it’s imperative that all documentation is up to date. But tracking the most current versions of documents — whether that’s research protocols, consent forms, disclosure statements, or other required forms — can be difficult when managed manually, leading to the use of outdated documents.
- Incomplete records — When you’re using paper forms, it’s much easier to skip required fields or fail to include supporting documentation, creating compliance gaps that can be difficult to track, and that may not be discovered until an audit.
Process inefficiencies and delays
Another issue with manually managing workflows in healthcare research is inefficiency — creating more work than is necessary. For example, manual processes can cause a host of needless and tedious issues, like:
- Time-consuming paperwork — With manual processes, researchers and managers can spend hours filling out, looking at, and processing forms. This time could be spent on real research.
- Approval bottlenecks — Paper-based approval processes are notorious for slowing progress. Why? Because they require documents to physically move from one approver to the next. It makes it hard to track where items are in the workflow. It also makes it much easier for things to slip through the cracks, like an approval sitting on someone’s desk for weeks, which makes the whole approval process take longer.
- Duplicative efforts — Without integrated systems, researchers often find themselves having to enter the same information multiple times across different forms and systems, which is not only a waste of time, but an increased risk for administrative errors.
- Followup challenges — Manual tracking of submission deadlines, required updates, approval signatures, and renewal timelines is both time- and labor-intensive, making it easy for things like a missed signature or form to fall through the cracks, leading to missed deadlines.
Audit and reporting difficulties
Compliance documentation that’s managed manually presents serious challenges for reporting and audits, including:
- Scattered documentation — With manual processes, important records may be spread across email inboxes, shared drives, paper files, and individual computers. This makes it very hard to quickly and efficiently put together all the required documentation for auditors.
- Limited audit trails — Manual processes rarely create comprehensive audit trails showing who reviewed or approved documents, when changes were made, or why certain decisions were reached, making the audit process significantly more challenging.
- Reporting challenges — Many healthcare research workflows require extensive reporting. But when data is manually compiled from multiple sources (both digital and physical), generating accurate reports becomes a huge time- and labor-intensive job. The resulting time crunch can pull your team away from more important work, causing productivity to drop.
- Remote access limitations — Paper-based and siloed electronic systems make it difficult for researchers, administrators, or external stakeholders to access necessary documentation when working remotely or across multiple sites — which not only makes everyone’s job more difficult, but also takes more time.
How workflow automation transforms research compliance management
The previous information has established that managing processes manually can make healthcare research workflows significantly more difficult and time-consuming. But the good news is there’s no reason to manage workflows manually! Workflow automation can address and solve all of these challenges, revolutionizing how healthcare research institutions manage disclosures, compliance, and documentation.
Standardized forms and submission processes
Automation can create consistency and support compliance in research and disclosure documentation in a number of different ways, including:
- Standardized digital forms — Automated systems provide standardized forms, ensuring all documentation is consistent and complete across the organization.
- Dynamic forms — Many automated systems allow you to create dynamic forms that adapt and change based on specific inputs, ensuring researchers are only shown relevant questions and fields based on their previous responses. This streamlines the process and saves researchers from reviewing irrelevant or unnecessary questions or forms.
- Data validation — Automated data validation can immediately flag missing information or inconsistencies, allowing researchers to correct the issue before submission, rather than requiring time-consuming revisions later in the process that could delay approval or acceptance.
- Prepopulated information — Systems can automatically pull existing information from institutional databases — for example, researcher credentials or standard institutional information — reducing redundant data entry and ensuring consistent formatting.
- Centralized form management — When forms need updating due to regulatory changes, rather than updating each form manually, automated systems allow for centralized updates that immediately deploy across the institution, which eliminates the risk of researchers getting their hands on outdated forms.
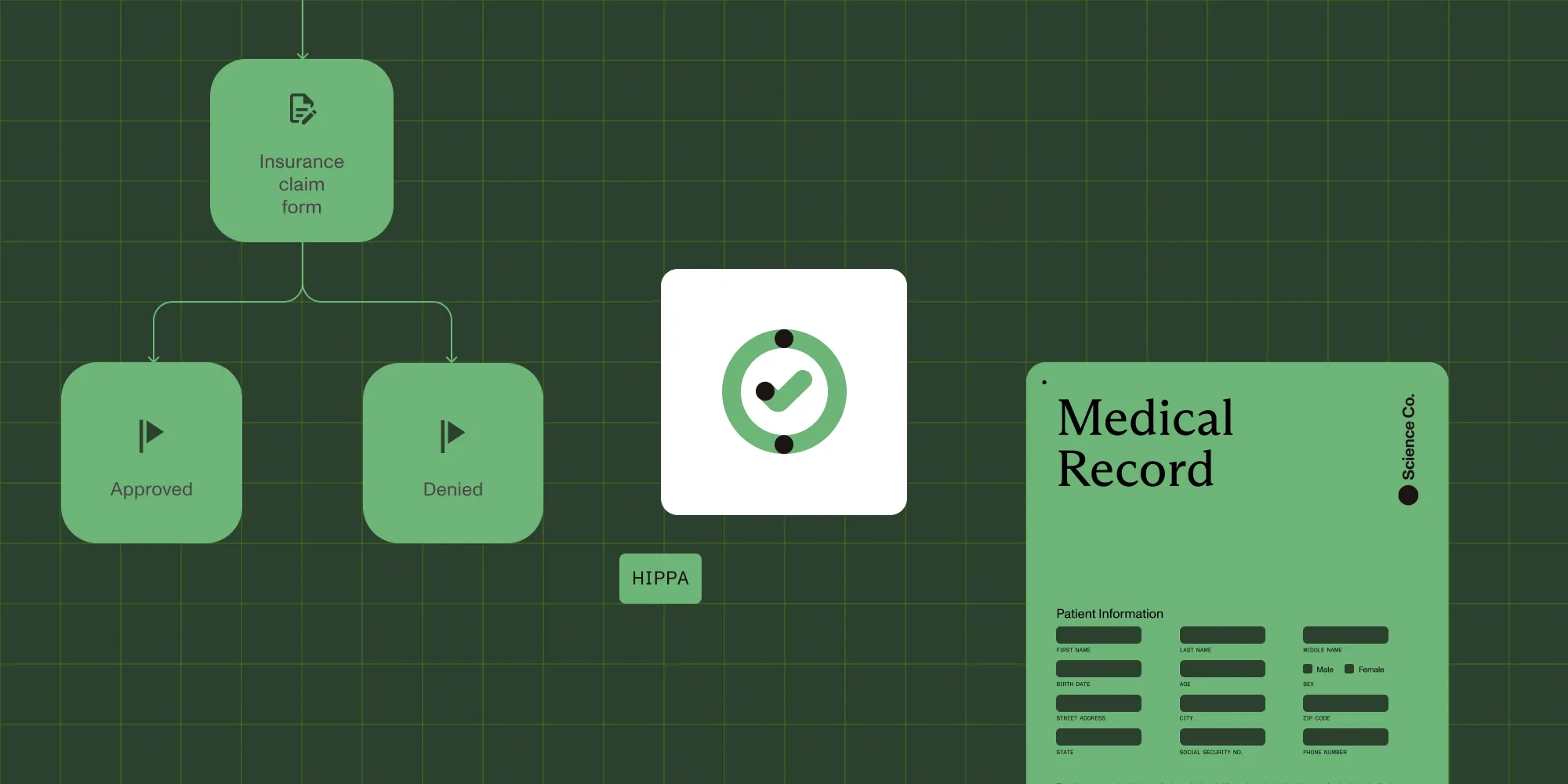
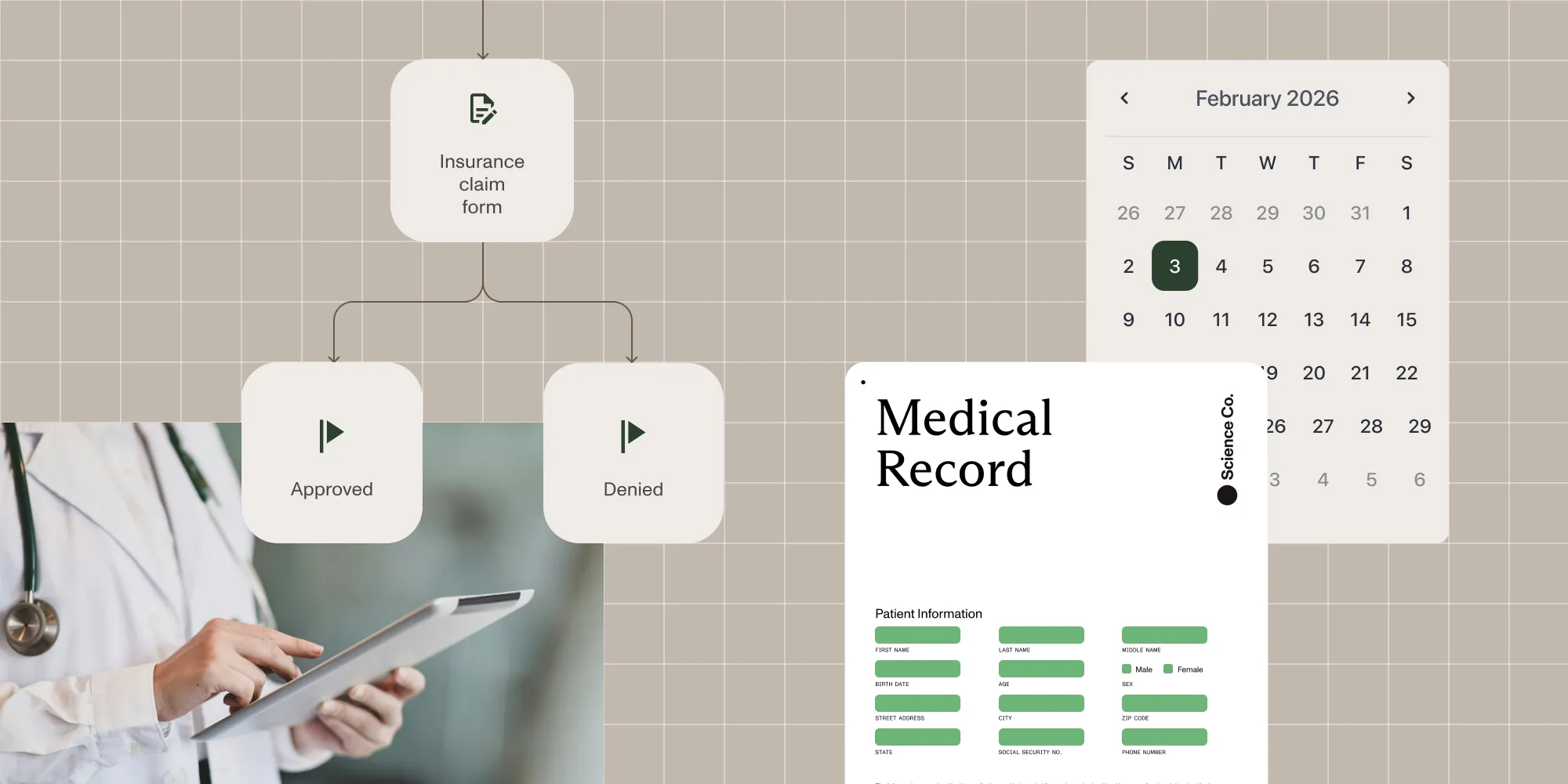
Streamlined approval workflows
Workflow automation can also dramatically improve the efficiency of research approval processes in a number of ways, including:
- Automated routing — With the right academic medical research compliance tools, documents automatically flow to the appropriate reviewers based on different variables, such as research type, risk level, department, or funding source. This eliminates manual handoffs, reducing approval time and minimizing bottlenecks.
- Parallel reviews — Automated systems also offer parallel reviews, which (when appropriate) allows multiple stakeholders to review documents simultaneously rather than one at a time — significantly reducing total approval time, while still ensuring all relevant stakeholders review and approve all documents.
- Reminder systems — Automated reminders inform reviewers of pending items and approaching deadlines, preventing bottlenecks caused by overlooked requests.
- Status tracking — With healthcare research workflow automation platforms, researchers and administrators can see exactly where submissions are in the approval process, which can eliminate uncertainty and reduce unnecessary followups.
- Exception handling — While approval processes have strict protocols, there may be exceptions. For example, if one approver is out of the office for an extended period (like a vacation or sick leave), approvals may need to be rerouted to an alternate approver. Automated systems can handle these exceptions, creating alternate approval paths, which can keep the approval process moving forward, even when primary reviewers are unavailable.
Comprehensive audit trails and documentation
Arguably, the biggest benefit of healthcare research workflow automation, at least from a compliance standpoint, is the comprehensive audit trail that it creates for IRBs, ethics boards, and sponsors.
- Complete revision history — Automated systems maintain a comprehensive record of every version of every document, showing what changed, who made the change, when it occurred, and even why it was made.
- Decision documentation — With many automated systems, reviewers can write down why they made changes or decisions. This makes it clear why changes were asked for or decisions were made.
- Access logging — Automated systems also keep records of everyone who accessed sensitive research documents — as well as when they accessed them — creating accountability and supporting security compliance.
- Timestamp verification — As mentioned, many disclosures and regulatory submissions have strict time requirements. With automated systems, electronic timestamps show when submissions, reviews, and approvals occurred, which creates proof that all documents were completed within the required timeframe.
- Automatic archiving — In addition to submission requirements, healthcare research institutions also need to comply with regulations around how — and how long — they store relevant documents. Automated systems can be configured to archive documents in compliance with all relevant institutional and regulatory retention requirements, ensuring nothing is lost, deleted too soon, or kept for too long.
Enhanced disclosure tracking
Workflow automation also significantly improves disclosure management and tracking through:
- Automated update reminders — Research disclosure tracking software can automatically notify researchers when disclosure updates are due, which ensures updates are completed on schedule.
- Relationship tracking — Automated systems can maintain comprehensive records of researcher relationships with outside entities, making it easier to identify potential conflicts for specific studies.
- Cross-reference capabilities — Automated systems can also cross-reference researcher disclosures with other study sponsors and flag potential conflicts that could be missed in a manual review.
- Disclosure verification — Electronic signature capabilities ensure disclosures are properly certified by researchers with clear documentation of when certifications were made, and by whom.
Potential applications of research workflow automation
Now that you understand the benefits of healthcare research workflow automation, this section provides an overview of some of the potential real-world applications.
There are a number of ways healthcare organizations and research institutions could implement automation into their workflows and reap the rewards that come along with it.
- Streamlined IRB submissions — Automated IRB submission workflows help researchers complete applications more accurately and route them to the appropriate reviewers, reducing review cycles and accelerating research timelines.
- Enhanced conflict of interest tracking — Research disclosure tracking software streamlines the process of collecting, updating, and monitoring financial and non-financial relationships, in turn helping institutions identify any potential conflicts of interest and maintain compliance.
- Workflow automation for clinical trials — Automation transforms clinical trial management by standardizing protocol documentation, tracking patient enrollment, managing case report forms, and coordinating between clinical staff and research teams.
- Coordinated multisite studies — Automated systems ensure consistent protocol implementation across all research sites, standardizing documentation and reporting processes, as well as ensuring all documentation is in compliance with each site’s regulations.
- Comprehensive audit readiness — Automated systems generate complete audit trails for IRBs, ethics boards, and sponsors, documenting every interaction with research protocols and supporting materials.
- Simplified adverse event reporting — Automation streamlines the complex process of documenting and reporting adverse events to appropriate oversight bodies, doing so quickly and within required timeframes.
- Efficient protocol amendment management — Workflow systems help track changes to research protocols, ensuring all stakeholders review and approve modifications, and then update protocols accordingly.
- Centralized document repositories — Automated systems maintain secure, centralized storage for all research documentation, making it easily accessible to authorized users when needed.
- Integrated grant compliance — Automation helps research teams track and meet the various documentation and reporting requirements from different funding sources, ensuring compliance, and keeping projects moving forward.
- Simplified researcher onboarding — Workflow automation also standardizes the process of training and credentialing new researchers, not only ensuring they meet all institutional and regulatory requirements, but also creating proof that they met those requirements.
Best practices for implementing research workflow automation
Considering using workflow automation to improve research workflows and disclosure tracking within your institution? Here are some best practices to keep in mind:
- Map your current processes first — Before selecting an automation solution, thoroughly document your existing research workflows, identifying pain points, bottlenecks, and compliance vulnerabilities. This mapping will help you prioritize which processes to automate first and ensure the workflow automation platform you choose addresses your specific needs.
- Start with high-impact processes — You may be tempted to automate everything at once, but if you want automation to be successful within your institution, it’s important to fight that temptation. Instead, start by choosing one or two processes that either cause the most pain or have the highest compliance risk, and start there. That’ll allow you to create real impact without overwhelming your team or changing too much at once.
- Choose research-specific solutions — Rather than going for a general workflow automation tool, opt for a platform designed specifically for research compliance, which often comes equipped with research-specific features such as IRB workflows and reporting capabilities that align with common regulatory requirements.
- Plan for integration — Whatever workflow automation solution you choose should integrate with any other institutional systems you rely on, like electronic medical records, grant management software, or credentialing databases. This will eliminate duplicate data entry, ensure consistency across systems, and make implementations significantly easier and more seamless.
- Measure success — When you start automating workflows, it’s important to measure the impact it has on your organization. Define the metrics that matter most to your organization — for example, error reduction, approval time reduction, or audit outcomes — and then track the impact workflow automation has on these metrics. The more you can prove that automation is positively impacting your workflows, the easier it will be to make a case for implementing it across other processes.
Your next step is to do your own research on how Nutrient Workflow Automation eases the pain points of your organization and teams. Try our solution free for 14 days to transform your research workflows now.