The future of healthcare document automation
Table of contents
Try Workflow Automation free for 14 days.
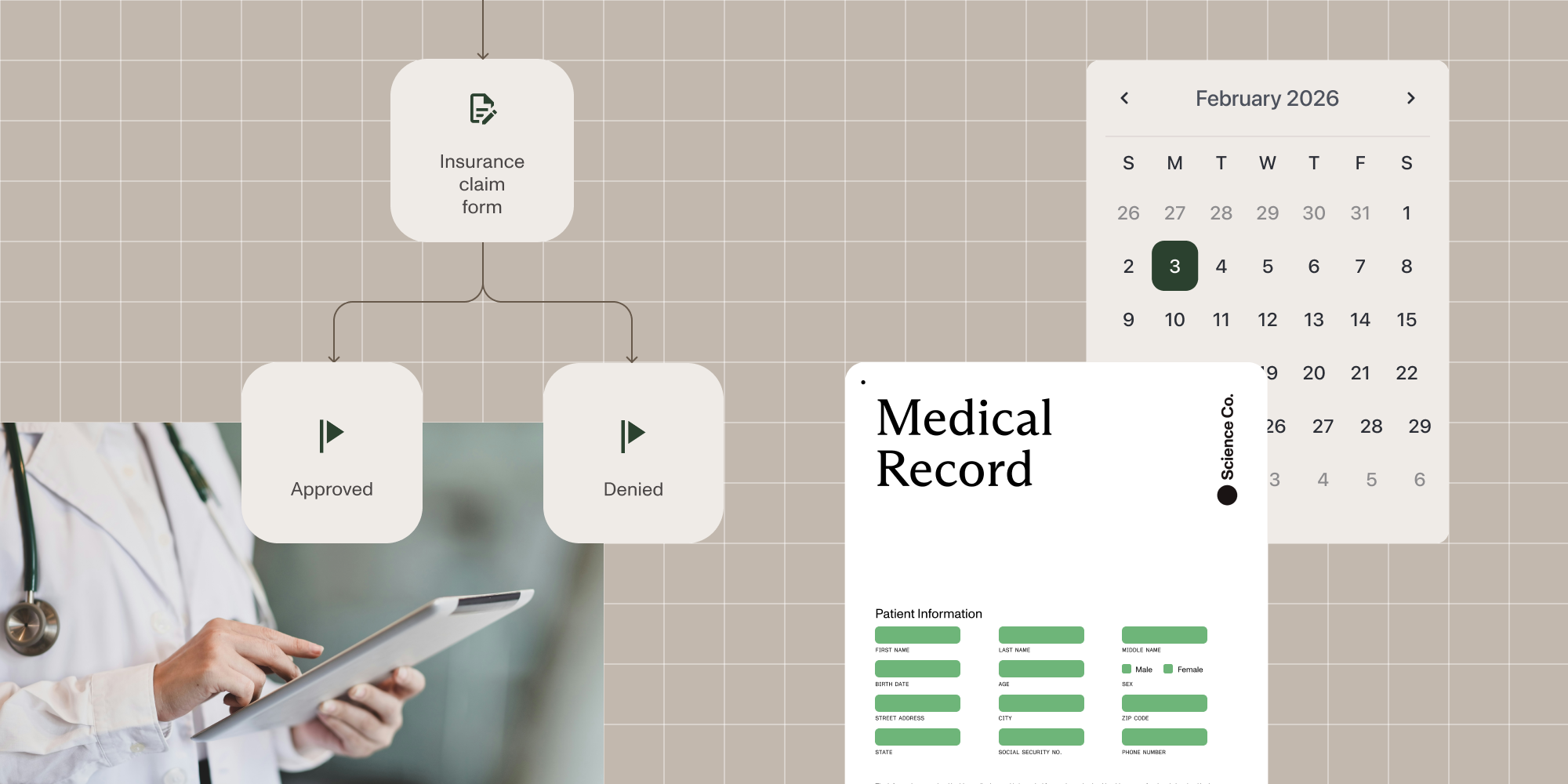
- Manual patient intake creates bottlenecks, data entry errors, and HIPAA compliance risks that compound across healthcare operations.
- Document automation cuts onboarding time by 60–70 percent, eliminates manual data entry, and embeds compliance controls directly into workflows.
- Nutrient Workflow Automation delivers HIPAA-compliant, no-code solutions that scale from single practices to enterprise health systems.
Healthcare depends on documents: patient intake forms, insurance verification, medical records, consent forms, billing paperwork. When these workflows rely on manual processes, healthcare providers hit predictable problems. Administrative bottlenecks. Data entry errors. Compliance risks. Staff burnout.
These problems compound. Delayed intake creates longer wait times. Missing forms delay billing. Compliance violations trigger regulatory penalties.
Healthcare organizations are automating document workflows out of necessity. Automated patient intake, records management, and document processing deliver faster throughput, fewer errors, and reliable HIPAA compliance.
We’ll examine the specific challenges of manual healthcare document management, the industry’s move toward automation, and how Nutrient Workflow Automation modernizes healthcare operations.
The pain of manual patient intake and records management
Manual document processes affect every department: front desk, billing, clinical staff, and patients.
Administrative bottlenecks
Front desk staff manage multiple documents per patient: intake forms, insurance cards, consent documents, medical history. Manual processing requires:
- Handing out forms and waiting for completion
- Verifying insurance by phone or computer
- Retyping handwritten information into systems
- Tracking down missing forms
- Filing or scanning into multiple systems
One delayed step backs up the entire schedule. Providers run late. Staff rush to catch up. Patient wait times increase.
Data entry errors and inconsistencies
Manual entry creates errors. Illegible handwriting becomes incorrect patient data. Staff rushing through paperwork make typos. Different team members use different formats, causing downstream problems.
The consequences are serious: Misidentified patients or incorrect dosages can cause medical errors, and billing mistakes trigger denials — according to the Medical Group Management Association (MGMA), around 30 percent of insurance claim denials stem from manual data entry errors — leading to lost revenue and time-consuming corrections. Incomplete or duplicate records slow clinical decisions and compromise patient safety.
Compliance and security risks
HIPAA governs how patient information is collected, stored, shared, and accessed. Manual processes create compliance gaps:
- Paper forms on desks expose protected health information (PHI).
- Faxes get misdirected.
- Access tracking remains unreliable.
- Staff training needs constant reinforcement.
- Audit trails stay incomplete.
HIPAA violations cost thousands to millions of dollars, and they also damage patient trust and organizational reputation.
Staff burnout and turnover
Administrative staff face constant pressure: high patient volumes, demanding physicians, frustrated patients, endless paperwork. When staff spend days copying information, chasing forms, and fixing errors, job satisfaction drops.
Burnout drives turnover; studies show healthcare administrative roles experience 20–35 percent annual turnover. As a result:
- Recruiting and training costs increase.
- Experienced staff take knowledge with them.
- New hires reduce productivity during ramp-up.
- Remaining staff shoulder extra work.
The pattern creates workforce instability and inconsistent service.
The macro shift toward workflow automation in healthcare
Manual document processes can’t scale with modern healthcare demands. Four trends drive automation adoption.
Rising patient volumes and expectations
Patient volumes keep growing. The U.S. population over 65 is projected to grow by 42 percent from 2022 to 2050(opens in a new tab), driving increased healthcare utilization alongside expanded insurance access and preventive care awareness.
Patient expectations have shifted too. People expect healthcare to match their digital banking experience: online forms before appointments, portal access to records, and clear billing communication.
Manual processes fail at this scale, and organizations clinging to paper forms lose patients to competitors with digital workflows.
Regulatory pressure and compliance requirements
Compliance requirements multiply beyond HIPAA. Examples of this include:
- State-specific privacy laws
- Medicare and Medicaid documentation requirements
- Insurance company reporting standards
- Quality reporting programs (MIPS, MACRA)
- Joint Commission accreditation standards
Manual processes can’t maintain this level of compliance. Automated workflows embed compliance checks directly into operations.
Technology advancement and integration capabilities
Modern automation platforms connect healthcare IT systems. Patient data entered once flows to:
- Electronic health record (EHR) systems
- Practice management software
- Billing systems
- Insurance verification platforms
- Appointment scheduling tools
Integration eliminates duplicate entry, reduces errors, and provides unified patient views.
Value-based care and operational efficiency
Healthcare payment models now reward outcomes over volume. Value-based care demands:
- Care coordination across providers
- Accurate data collection and reporting
- Patient engagement and communication
- Resource efficiency to control costs
Workflow automation enables these requirements through streamlined operations, data accuracy, and staff reallocation to patient education and care coordination.
How document automation transforms healthcare operations
Document automation impacts three operational metrics: speed, accuracy, and compliance.
Speed: Faster patient onboarding and processing
Automated intake cuts onboarding time for new and returning patients.
Before automation — Patients arrive 15–20 minutes early for paper forms. Staff manually enter data. Insurance verification requires phone calls. Total time: 20–30 minutes before seeing the provider.
After automation — Patients complete forms online before appointments. Data flows directly into practice systems. Insurance verification runs automatically. Patients confirm information and see providers within minutes.
The result — 60–70 percent reduction in onboarding time. Providers see more patients without extending hours or adding staff.
Accuracy: Eliminating errors and ensuring data quality
Automation removes manual data entry and its errors.
Patients enter their own information, eliminating handwriting and transcription problems. Validation rules catch invalid insurance numbers and missing fields before submission. Data flows automatically to all systems, maintaining consistency.
Results: Accurate medical records. First-time-right billing claims. Reliable quality reporting. Staff time shifts from error correction to productive work.
Compliance: Strengthening HIPAA compliance and security
Automated workflows embed HIPAA compliance into document processes.
Access controls: Role-based permissions restrict patient information access. Every attempt gets logged.
Audit trails: Complete logs show who accessed information and when, as well as what changed. Supports compliance reporting.
Secure transmission: Encryption protects PHI in transit and at rest across all systems and storage.
Automated checks: Workflow rules enforce requirements like two-factor authentication or access expiration.
Automation also reduces human-caused violations. Systems enforce secure messaging. Role-based controls prevent unauthorized access.
Signs your healthcare organization is ready for document automation
Seven indicators signal readiness for automation.
- High patient volume creating bottlenecks: Full waiting rooms, overwhelmed front desk staff, and patient complaints about wait times point to intake bottlenecks. Administrative tasks can’t match patient volume.
- Staff spending significant time on data entry: Track staff time allocation. If they’re rekeying form data into systems, you’re paying for work computers do better.
- Frequent billing delays or claim denials: Regular claim denials from incorrect or incomplete information indicate data quality problems. Missing documentation and entry backlogs delay billing.
- Compliance concerns or audit findings: HIPAA violations, audit gaps in access controls, incomplete audit trails, or inconsistent documentation show manual processes failing compliance requirements.
- Patient complaints about administrative experience: Satisfaction surveys mentioning frustrating paperwork, long waits, or repetitive information requests reveal process problems.
- Staff burnout and turnover: High administrative turnover with exit interviews citing workload or satisfaction issues points to tedious manual work.
- Difficulty scaling operations: When you can’t grow because administrative processes are maxed out, automation enables scaling without proportional staff increases.
How Nutrient modernizes healthcare workflows
Nutrient shapes healthcare document automation through a comprehensive, no-code platform that streamlines clinical, administrative, and compliance documentation workflows.
End-to-end document automation
Nutrient eliminates manual data entry and paperwork by automatically generating documents directly from EMR, EHR, and healthcare data sources:
- Patient visit summaries
- Informed consent forms
- Compliance reports
- Insurance claims
- Patient education materials
- Discharge instructions
Documents generate automatically, reducing errors, accelerating processes, and maintaining consistency across all patient documentation. Staff spend less time on paperwork and more time on patient care.
No-code workflow builder
Healthcare teams design and deploy custom document workflows without IT resources or coding skills. The intuitive drag-and-drop interface empowers non-technical staff to create and modify workflows independently:
- Clinical staff build patient intake workflows matching their exact processes.
- Billing departments automate claims processing based on payer requirements.
- Compliance officers create audit documentation meeting current regulations.
- Department managers standardize procedures across their teams.
- Administrative staff adapt forms and routing without submitting IT tickets.
This democratizes automation. Teams adapt quickly to changing regulatory requirements or operational needs without waiting for IT projects. When Medicare changes documentation requirements or a new insurance verification process launches, your staff updates workflows the same day.
HIPAA and regulatory compliance
The platform meets HIPAA and healthcare-specific regulations through built-in security controls:
Encrypted storage and transmission — PHI remains encrypted at rest and in transit across all systems and workflows.
Role-based access controls — Granular permissions restrict patient information access by job function and clinical role.
Comprehensive audit logging — Every action gets tracked and timestamped. View who accessed records and when, and what changes they made.
Compliance reporting — Prebuilt reports demonstrate regulatory compliance for audits and assessments.
Your automated workflows meet regulatory requirements from implementation. Compliance documentation for audits takes minutes instead of weeks.
Configure once, deploy everywhere
Nutrient’s solutions scale across departments, locations, and use cases:
Template library — Build workflows once, and then replicate across multiple facilities or departments with location-specific customization.
Multisite deployment — Healthcare systems can standardize processes across all locations while allowing site-specific variations.
Cross-departmental coordination — Patient data flows seamlessly from intake through discharge, connecting admissions, clinical care, billing, and case management.
Growth accommodation — Cloud architecture scales from single practices to enterprise health systems without performance degradation or costly migrations.
Advanced healthcare features
Purpose-built capabilities address specific healthcare documentation needs:
Electronic signatures — HIPAA-compliant eSignatures enable remote consent, authorization, and approval workflows.
Conditional logic — Documents adapt based on patient data, treatment types, insurance coverage, or clinical pathways. Generate only relevant sections.
Collaborative review — Multiple providers can review, annotate, and approve documents simultaneously with full audit trails of all changes.
These features combine to reduce administrative burdens, improve compliance consistency, and free healthcare teams to focus on patient care.
Getting started with healthcare document automation
Below are five steps to implement automation successfully.
Assess your current processes
Document existing workflows: patient intake, records requests, billing documentation. Map each step. Identify pain points, bottlenecks, and compliance gaps. This baseline helps prioritize automation targets.
Define success metrics
Set measurable targets:
- Intake processing time reduction
- Data entry error rates
- Claim denial rates
- Staff administrative time
- Patient satisfaction scores
- Compliance audit findings
Quantifiable goals demonstrate ROI and guide priorities.
Start with high-impact workflows
Focus initial automation on one or two workflows:
- Patient intake touches every patient and shows immediate results.
- Insurance verification delivers measurable time savings.
- Consent management addresses critical compliance.
Early wins build confidence for broader automation.
Ensure HIPAA compliance from day one
Choose vendors with healthcare expertise. Verify:
- Business associate agreements (BAA) meeting HIPAA standards
- Security features protecting PHI
- Audit capabilities supporting compliance reporting
- Healthcare organization experience
Build compliance into automation strategy from the start.
Train staff and manage change
Successful automation needs change management:
- Explain automation benefits for staff.
- Train thoroughly on new workflows.
- Designate workflow champions.
- Gather feedback and adjust.
- Share success stories.
Staff who see automation making work easier become change advocates.
The competitive advantage of healthcare document automation
Document automation creates sustainable competitive advantages.
Modernized organizations can:
- See more patients — Without extending hours or adding staff, increasing revenue without proportional costs
- Improve patient satisfaction — Through streamlined experiences, driving loyalty and referrals
- Reduce operational costs — By eliminating manual processes and errors; automation could save the U.S. healthcare system an estimated $20+ billion annually(opens in a new tab)
- Attract and retain talent — With modern work environments focused on meaningful tasks
- Strengthen compliance — Through built-in controls, reducing violation risk
- Scale operations — Efficiently without administrative bottlenecks
These advantages compound. The performance gap between automated and manual providers widens over time.
FAQ
Most organizations see initial workflows live within 2–4 weeks. The timeline depends on workflow complexity and your existing IT infrastructure. A typical implementation follows this schedule:
- Week 1 — Workflow assessment and configuration planning
- Week 2–3 — Workflow building and integration testing
- Week 4 — Staff training and pilot launch
Because Nutrient’s no-code platform empowers non-technical staff, you can continue building and refining workflows after initial launch without waiting for IT resources.
HIPAA compliance is built into the platform through multiple layers of security and documentation:
- Business associate agreements — Nutrient signs BAAs with all healthcare customers
- Encryption — PHI is encrypted at rest and in transit using industry-standard protocols
- Access controls — Role-based permissions restrict data access by job function
- Audit logging — Complete, immutable logs track who accessed what data and when
- Compliance reporting — Prebuilt reports demonstrate adherence to HIPAA requirements
The platform meets HIPAA and state-specific privacy regulations. Our Trust Center(opens in a new tab) provides detailed security documentation and SOC 2 reports.
You control the migration pace. Most organizations use a phased approach:
- Digital duplication — Run paper and digital forms in parallel initially
- Gradual transition — Move one workflow at a time (start with new patient intake)
- Paper phaseout — Eliminate paper once staff are comfortable with digital processes
- Archive conversion — Optionally digitize existing paper records using OCR
Your existing paper forms can be recreated digitally, maintaining familiar layouts while adding validation and automation. Staff don’t need to learn entirely new processes — they’re using improved versions of familiar workflows.
No. The no-code workflow builder is designed for clinical and administrative staff to use independently:
- Drag-and-drop interface — Build workflows visually without coding
- Prebuilt templates — Start with healthcare-specific templates for common workflows
- Real-time testing — Preview workflows before deploying them
- Easy modifications — Frontline staff can update forms and routing rules as needs change
IT involvement is typically limited to initial EHR integration setup. After that, department staff manage their own workflows. When Medicare updates documentation requirements or insurance processes change, your team adjusts workflows immediately without submitting IT tickets.
Most healthcare organizations see ROI within 6–12 months through:
- Labor cost reduction — Less time on data entry and paperwork means the same staff can handle higher patient volumes
- Revenue acceleration — Faster, more accurate billing reduces claim denials and speeds payment collection
- Penalty avoidance — Better compliance reduces HIPAA violation risk
- Efficiency gains — 60–70 percent reduction in intake time translates to more patient appointments
While automation requires upfront investment (software licensing, implementation, training), the ongoing savings from eliminated manual work typically exceed costs within the first year. For specific pricing, contact our Sales team for a customized quote based on your organization size and requirements.
Change management is critical for successful automation. Address resistance through:
Early involvement — Include frontline staff in workflow design so they help create solutions rather than having changes imposed on them.
Clear benefits communication — Show staff how automation eliminates frustrating tasks they currently handle manually: no more chasing missing forms, rekeying data, or fixing errors.
Adequate training — Provide hands-on training sessions where staff practice with the new system before going live.
Workflow champions — Designate enthusiastic early adopters to support colleagues and share success stories.
Gradual rollout — Start with one simple workflow to build confidence before tackling complex processes.
Staff who initially resist often become the strongest advocates once they experience how much easier automation makes their daily work. The key is demonstrating concrete benefits rather than just mandating change.
Taking the next step
Manual intake and records management limit healthcare providers. The industry adopts automation for clear benefits: faster processing, fewer errors, stronger compliance.
Organizations with high patient volumes, compliance challenges, staff burnout, or scaling needs should automate now. The technology exists. Waiting costs more each day.
Nutrient Workflow Automation delivers:
- A HIPAA-compliant platform with security and audit capabilities
- 60–70 percent reduction in patient onboarding time
- Integration with existing healthcare IT systems
- Scalability matching organizational growth
Healthcare document management will be automated, secure, and efficient. The only question is when your organization makes the switch.
Ready to modernize your healthcare workflows? Contact our Sales team to discuss your requirements and see Nutrient Workflow Automation in action.
Learn more about healthcare workflow automation solutions or explore how workflow automation transforms business operations.